
Misconceptions:
Osteoporosis and BMD
If you didn't have bones you would just be a shapeless blob on the floor. You might have learned about human skeleton from the popular song "that the ankle bone is connected to knee bone..." etc you might have been taught by your parents, teachers and doctors to drink milk to build strong bones and teeth.
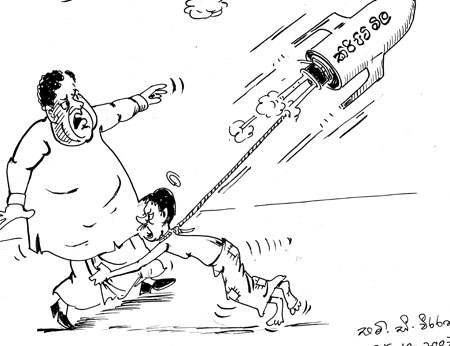
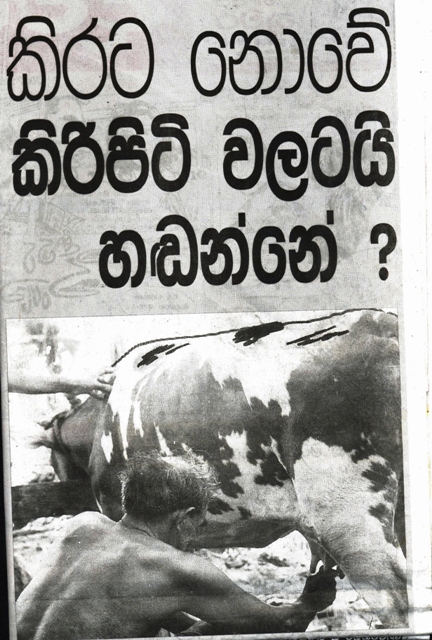
You must have watched a lot of television advertisements (TV ads) and ads in newspapers and journals giving you all the beneficial effects of various brands of malted milk and (cow's) milk powder and how these various brands of malted milk and cow's milk containing varying amounts of calcium prevent osteoporosis.
Americans consume more cow's milk and its products than most populatations in the world. So Americans must have wonderful strong bones. Unfortunately this is not so. A recent study showed that American women aged 50 and older have one of the highest rates of hip fractures in the world.
The only countries with higher rates of hip fractures are in Europe and in South Pacific (
An excess rate of hip fractures often used as a reliable indicator of osteoporosis, a bone disease which especially affects women after menopause and this is claimed to be due to inadequate intake of calcium.
Dairy products are particularly rich in calcium, so that dairy industry eagerly supports efforts to boost calcium consumption. This is why you see so many TV ads about various brands of milk powder and malted milk. As mentioned earlier these countries that use the most cow's milk and its products also have the highest fracture rates and worst bone health.
One possible explanation is found in a report showing an impressively strong association between intake of animal protein and bone fracture rate for women in different countries.
Authored in 1993 by researchers at Yale University School of Medicine, the report summarized data on protein intake and fracture rates taken from 34 separate surveys in 16 countries that were published in 29 peer - reviewed publications. All the subjects in these surveys were women 50 years and older and it is noteworthy that 70 percent of the fracture rate was attributable to consumption of animal protein.
These researchers explained that animal protein unlike plant protein increased the acid load in the body. The body does not like this acidic environment and begins to fight it. In order to neutralize the acid, the body uses calcium which acts as a very effective base.
This calcium must come from somewhere and it ends up being pulled from bones and the calcium loss weakens the bone, putting them at greater risk for fracture.
There had been evidence for well over 100 years that animal protein decreases bone health. In 1880 it was first suggested that animal protein causes metabolic acid load and this was documented as long as 1920 and other studies showed that consumption of animal protein is more effective than plant protein at increasing metabolic acid load in the body.
When animal protein increases metabolic acid and draws calcium from bones, amount of calcium in urine is increased and average American intake of protein is 70-100g/day. The observation on the association between animal protein consumption and bone fracture rate is very impressive.
A study published in 2000, comes from the department of Medicine, at the
The study of Osteoporotic Research Group at
In rural
Do widely advertised claims that protein-rich dairy products protect our bones? Everyday we watch TV ads showing advantages of taking certain brands of milk powder containing calcium to get strong bones and to prevent osteoporosis.
It would be very interesting for one of our orthopaedic surgeons or a rheumatologist to compare the incidence of hip fractures among rural post menopausal women (who consume less animal proteins than the urban women) with urban post menopausal women who consume more animal proteins and takes calcium tablets regularly.
Prof. Mark Hegsted (long time Harvard Professor) believes that excessive high intake of calcium consumed over a long time impairs the body's ability to control how much calcium it uses and when.
Under healthy conditions the body uses an activated form of vitamin D, "calcitirol" to adjust how much calcium it absorbs from food and how much it excretes and distributes in the bones. Calcitriol is considered a hormone. It seems perfectly plausible that animal protein and even calcium when consumed at excessive levels are capable of increasing the risk of osteoporosis.
But dairy industry still suggests that we should consume more of its products and spends hundreds of thousands of rupees to advertise their products with a view to built strong bones and teeth. Huge amounts of money are at stake as well.
One of the most cited osteoporosis experts, one funded by dairy industry angrily wrote in a prominent editorial, that the diet favouring a diet with higher ratio of plant-to-animal protein cited above could have been influenced to some extent by 'currents' in the larger society (The currents he was referring were animal rights activitists opposed to the use of dairy foods).
Bone Mineral Density (BMD)
BMD is a measure of bone density that is often used to diagnose bone health. If BMD falls below a certain level you may be at risk of osteoporosis i.e., if your BMD is low, you are at a risk for fracture.
Much better predictor of osteoporosis is dietary ratio of animal-to-plant protein the higher the ratio higher the risk of disease. BMD appears as it is associated with the ratio.
The researchers believe that the problem may be due to the effects of calcification and bone like formations in blood vessels Vit. D. enhances calcium absorption. Current dietary calcium and Vitamin D recommended for adult over 50 years of age are 1,200 mg and 400 to 600 i.u. respectively and recent findings suggest that these recommendations may be too high for general population.
The WHO acknowledges that less dietary calcium is needed when animal protein consumption is low.
Risk of osteoporosis
1) Stay physically active. Take the stairs instead of the lift; Brisk walking daily for about one hour or jogging, cycling or swimming or doing yoga are useful measurers.
2) Eat a variety of whole plants foods, avoid animal foods; calcium is available in plenty in plant foods such as "Niwithi", legumes such as beans and leafy vegetables. Stay away from refined carbohydrates like sugary cereals, candies, plain pastas and white breads.
3) Keep your salt intake to a minimum. Avoid highly processed and packaged foods which contain excess salt.
4) Don't be deceived by misleading TV ads about milk foods which the dairy industry claims to prevent osteoporosis.
.jpg)






















1 comment:
This is a really good site post, i am delighted I came across it. I will be back down the track to check out other posts that
milk supply supplements
Post a Comment